Stroke is a leading cause of death and long-term disability in Asia. The region bears more than half of the global stroke burden, fueled by high rates of hypertension, diabetes, smoking, and aging populations. This article examines the epidemiology of stroke in Asia, major risk factors, emergency treatment protocols, long-term rehabilitation, and strategies to reduce the devastating health and economic impact of stroke.

Stroke: A Growing Public Health Challenge in Asia
- Global burden: Over 12 million strokes occur annually, with 6.5 million deaths worldwide.
- Asian share: More than 60% of stroke cases and deaths occur in Asia.
- Disability impact: Stroke is the leading cause of disability-adjusted life years (DALYs) lost in Asia.
- Economic cost: Long-term rehabilitation and loss of productivity pose significant challenges.
Types of Stroke
- Ischemic Stroke (85%): Blockage of blood flow due to a clot.
- Hemorrhagic Stroke (15%): Rupture of a blood vessel in the brain, more common in Asia than the West.
- Transient Ischemic Attack (TIA): “Mini-stroke” warning of future major stroke.
Major Risk Factors in Asia
1. Hypertension
- The most significant risk factor for stroke in Asia.
- Poor control of high blood pressure leads to both ischemic and hemorrhagic strokes.
2. Diabetes
- Asia has the highest diabetes prevalence globally, greatly increasing stroke risk.
3. Smoking and Alcohol
- High smoking rates in China, India, and Southeast Asia.
- Excessive alcohol consumption associated with hemorrhagic stroke.
4. Diet and Lifestyle
- High-salt diets contribute to hypertension.
- Sedentary lifestyles due to urbanization.
5. Air Pollution
- Chronic exposure to fine particulate matter (PM2.5) linked to higher stroke incidence.

Symptoms of Stroke
- Sudden weakness or numbness in face, arm, or leg (especially one side).
- Difficulty speaking or understanding speech.
- Sudden vision problems.
- Severe headache with no known cause.
- Loss of balance, dizziness, or coordination.
FAST test:
- Face drooping
- Arm weakness
- Speech difficulty
- Time to call emergency services
Emergency Care and Acute Management
- Ischemic Stroke Thrombolysis: Intravenous tPA within 4.5 hours of onset. Mechanical thrombectomy: For large-vessel occlusion, effective up to 24 hours in select patients.
- Hemorrhagic Stroke Blood pressure control to reduce bleeding. Surgical interventions for hematoma removal. Intensive care support for brain swelling.
- Stroke Units Specialized hospital units significantly reduce mortality. Limited availability in rural Asia.
Rehabilitation and Long-Term Care
- Physical therapy: Restoring mobility and balance.
- Occupational therapy: Regaining independence in daily tasks.
- Speech therapy: For language and swallowing difficulties.
- Psychological support: High rates of post-stroke depression in Asia.
- Community rehabilitation: Support groups and home-based care.
Prevention Strategies
- Primary Prevention Hypertension and diabetes control. Smoking cessation campaigns. Promoting exercise and healthy diets.
- Secondary Prevention Antiplatelet therapy (aspirin, clopidogrel). Statins for cholesterol management. Anticoagulation for atrial fibrillation patients.
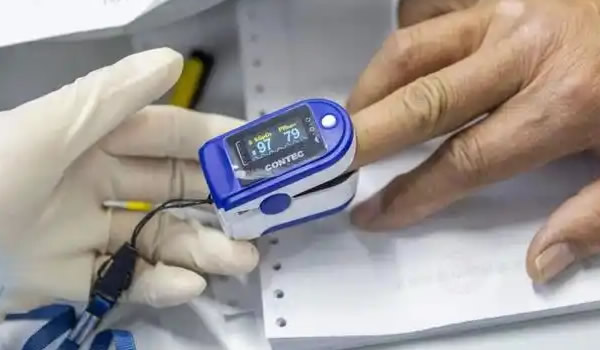
- Public Health Approaches Stroke awareness campaigns to recognize early signs. Subsidized blood pressure monitoring and screenings. Training first responders and community health workers.
Regional Insights
- China: Largest stroke burden globally; high hypertension and smoking prevalence.
- India: Increasing strokes in younger populations due to diabetes and lifestyle changes.
- Japan: Historically high hemorrhagic stroke rates, now reduced through national salt-reduction policies.
- Southeast Asia: Lack of stroke units in rural areas limits acute care.
- South Korea & Singapore: Advanced stroke care networks and strong rehabilitation systems.

Future Directions
- AI and mobile apps: Early stroke detection through speech and facial recognition.
- Telestroke programs: Remote neurologist support in rural hospitals.
- Wearables: Monitoring heart rhythm to detect atrial fibrillation.
- Robotics in rehab: Assisting mobility recovery.
- Policy focus: Expanding stroke units, insurance coverage for rehabilitation.
Conclusion
Stroke in Asia represents a public health emergency, with devastating consequences for individuals, families, and economies. Despite medical advances, late hospital arrivals, poor awareness, and inadequate infrastructure remain major barriers.
The key to reducing stroke burden lies in prevention, early recognition, timely emergency care, and comprehensive rehabilitation. With a coordinated regional approach—combining policy, technology, and community engagement—Asia can reduce the impact of stroke and improve outcomes for millions of patients.
stroke Asia, stroke prevention, emergency stroke care, stroke rehabilitation Asia