Stroke is one of the leading causes of death and disability in Asia, with an enormous healthcare and economic burden. The region carries a disproportionately high share of global stroke cases, often with younger age of onset, higher fatality, and worse functional outcomes compared to Western countries. This article explores stroke epidemiology in Asia, prevention strategies, acute care approaches, and rehabilitation methods that can reduce mortality and improve recovery.
Stroke: A Major Health Crisis in Asia
- Global impact: Stroke is the second leading cause of death worldwide.
- Asia-specific burden: Over 60% of global stroke cases occur in Asia.
- High mortality: Stroke deaths are particularly high in China, India, and Southeast Asia.
- Younger onset: In Asia, strokes often occur 10 years earlier than in Western populations.
- Economic impact: Stroke is a leading cause of long-term disability, straining families and healthcare systems.
Types of Stroke
- Ischemic stroke (80–85%): Caused by blood clots blocking brain arteries.
- Hemorrhagic stroke (15–20%): Caused by rupture of brain blood vessels, more common in Asia than in the West.
- Transient Ischemic Attack (TIA): “Mini-stroke” with temporary symptoms, a warning sign of future major stroke.
Risk Factors in Asian Populations
- Hypertension: Leading risk factor; poorly controlled in many Asian countries.
- Diabetes: High prevalence in South and East Asia.
- Smoking and betel nut use: Common in South and Southeast Asia.
- High salt diet: Linked with hypertension, especially in China and Korea.
- Atrial fibrillation: Increasingly important with aging populations.
- Obesity and sedentary lifestyles.
- Genetic susceptibility: Asians have higher risk of intracerebral hemorrhage.
Symptoms of Stroke
⚠️ Recognizing stroke early is vital. The FAST rule:
- Face drooping
- Arm weakness
- Speech difficulty
- Time to call emergency
Other signs include sudden vision problems, dizziness, severe headache, and confusion.
Prevention Strategies
1. Primary Prevention
- Blood pressure control: Community programs to screen and treat hypertension.
- Diabetes management: Affordable access to medications and lifestyle interventions.
- Smoking cessation and alcohol moderation.
- Dietary changes: Reduce salt, increase fruits, vegetables, and whole grains.
- Exercise promotion: At least 150 minutes of moderate activity weekly.
2. Secondary Prevention
- Antiplatelet therapy: Aspirin, clopidogrel for ischemic stroke survivors.
- Anticoagulation: For atrial fibrillation patients (DOACs increasingly used).
- Statins: Lower cholesterol and reduce stroke recurrence risk.

Acute Stroke Care
1. Stroke Units
- Dedicated hospital units improve survival and recovery.
- Still limited in many parts of Asia, especially rural areas.
2. Thrombolysis (tPA therapy)
- Intravenous clot-busting drug within 4.5 hours of ischemic stroke onset.
- Underutilized in Asia due to late hospital arrival and lack of trained staff.
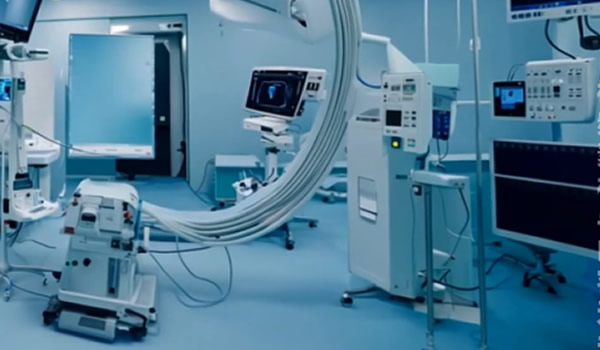
3. Mechanical Thrombectomy
- Removing clots via catheter-based procedure, effective up to 24 hours in some patients.
- Available mainly in urban hospitals in Japan, China, Singapore, South Korea.
4. Hemorrhagic Stroke Management
- Blood pressure control critical.
- Surgical interventions may be required for hematoma evacuation.
Stroke Rehabilitation
- Multidisciplinary approach: Physicians, physiotherapists, occupational therapists, speech therapists, psychologists.
- Early mobilization: Improves outcomes.
- Physical therapy: Strength and balance training.
- Speech therapy: For patients with aphasia or swallowing problems.
- Cognitive rehabilitation: Helps with memory and problem-solving issues.
- Community-based rehabilitation: Essential in resource-limited Asian settings.
Long-Term Care and Support
- Home care programs: Reduce hospital readmissions.
- Tele-rehabilitation: Increasingly used in Asia with mobile and AI tools.
- Psychological support: Depression common post-stroke; counseling helps recovery.
- Family involvement: Training caregivers improves outcomes and reduces burden.
Regional Perspectives
- China: Largest number of stroke cases globally; rapid expansion of stroke units.
- India: High burden, limited acute care infrastructure in rural regions.
- Japan & South Korea: Advanced stroke care systems with high rates of thrombolysis and thrombectomy.
- Southeast Asia: Rising burden with younger onset; prevention programs urgently needed.

Future Directions
- AI-based stroke detection: Mobile apps analyzing facial asymmetry and speech.
- Wearable devices: Monitoring heart rhythms to detect atrial fibrillation early.
- Regional stroke networks: Sharing expertise and emergency transfer systems.
- Precision medicine: Genetic and biomarker-driven stroke prevention strategies.
Conclusion
Stroke is one of Asia’s most pressing health challenges, causing widespread disability and death. Yet with prevention, timely acute care, and strong rehabilitation systems, outcomes can be significantly improved.
The path forward requires a coordinated effort—public health campaigns, investment in stroke units, accessible rehabilitation, and adoption of digital health innovations. By addressing stroke comprehensively, Asia can reduce its devastating human and economic toll.
stroke Asia, stroke prevention, acute stroke care, stroke rehabilitation Asia